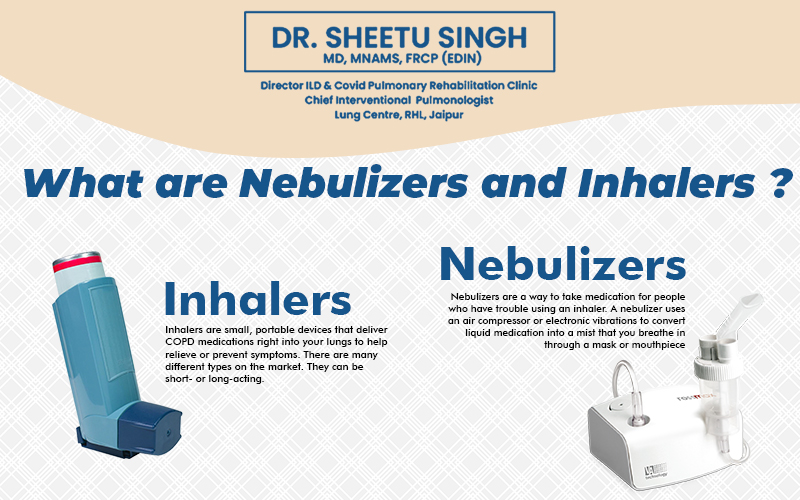
Nebulizers and Inhalers are tools that help kids take their Asthma medicines. Most asthma medications must be inhaled into the lungs for them to function as intended. Nebulizers are devices that change liquid medication into a mist for children to inhale. Often, inhalers—also known as puffers—dispense the medication as a spray. Some inhalers release the medicine as a fine powder. These tools are effective when used properly. But each has its pros and cons- so consult with Dr. Sheetu Singh about which one is best for your child.
1. InhalersThese compact, portable gadgets spray a dose of medication directly into your lungs. There are three basic types:
- Hydrofluoroalkane inhalers (HFA, formerly metered dose inhalers or MDI)
- Dry powder inhalers (DPI)
- Soft mist inhalers (SMI)
HFAs contain a liquid medication that you get through an Aerosol spray. The medication is contained in a metering valve-equipped pressurized canister. Breathe in carefully while applying pressure to the inhaler while sealing your lips around the mouthpiece or holding it one to two inches away from your lips. Many people like to use a spacer. The mouthpiece and the medication canister are connected via a hollow plastic tube. Using a spacer facilitates the delivery of the entire drug dose to your lungs.
A DPI is similar to an HFA, but it releases a puff of dry powder instead of a liquid mist. A DPI and a spacer shouldn’t be combined. Inhale quickly and steadily instead by firmly sealing your lips around the DPI inhaler’s mouthpiece. To prevent damp air from getting inside the device and causing the powder to clump, it’s crucial to take the device out of your mouth before exhaling.
An SMI is a more recent kind of inhaler that gives you a precise dosage in a slow-moving mist to make it easier for you to inhale the medication. You put your lips on the mouthpiece while you hold the device horizontally. Be careful not to cover the air vents. This kind of equipment actively administers medication without relying on the rate at which you breathe in the inhaled air. Despite sharing a common operating principle, inhalers operate differently. An HFA, for example, should always be shaken before use, yet a DPI should never be shaken.
2. NebulizersThese devices turn a liquid medication into a mist that you breathe in. You maintain a nebulizer at home as they are not particularly portable. The medicine is measured out into a cup for use, and the cup is connected to the machine via tubing. Next, activate it, unwind, and inhale deeply via a mouthpiece or mask as you take in the mist. Depending on the medication, it usually takes 20 minutes or less to inhale the medicine. Before using the nebulizer and mouthpiece or mask again, you must first clean them with water (and occasionally soap).
How Does an Inhaler Work?
- Metered Dose Inhaler (MDI)
A pre-measured spray of asthma medication is released by MDIs. They resemble miniature aerosol cans. A precise “puff” of medication is emitted when the inhaler is squeezed. MDIs require coordination when used on their own. A child needs to be able to inhale and trigger the device simultaneously. If not, the medication can find its way into the mouth as opposed to the lungs. That’s why many doctors recommend attaching the metered dose inhaler to a spacer.
A spacer functions as a sort of storage tank for asthma medication. On one end, it is attached to the inhaler, and on the other, it is attached to a mouthpiece or mask. The medication remains in the spacer until the user presses down on the inhaler, at which point they can inhale it. Hence, since all they need to “do” is sit and breathe, infants and very young children can take their medications using a metered dose inhaler with a spacer. It typically takes less than 30 seconds to provide medication to the lungs using a spacer.
There are counters on certain MDIs that show how many doses are left. To ensure that the inhaler is replaced on schedule, if there isn’t a counter, the number of doses already taken should be kept track of.
- Dry Powder Inhalers (DPI)
Dry powder inhalers deliver medicine as a powder. Additionally, the powder is inhaled, but it is not sprayed out. Youngsters must exert greater effort by rapidly and forcefully breathing the powdered medication. Most kids can do this when they’re around 5 to 6 years old. Dr. Sheetu Singh tends to prescribe MDIs more commonly than dry powder inhalers.
How Does a Nebulizer Work?
A nebulizer is a battery-powered or an electric machine. It usually has four parts:
- The motor.
- The mouthpiece or facemask.
- The cup.
- Tubing.
The cup, which has tubing connecting it to the motor, is filled with medication. The mouthpiece or facemask is then attached to the cup. The machine emits a mist into the mask when it is turned on. This mist allows the child to breathe.
Children just need to stay motionless and breathe to get the medication. It usually takes about 5 or 10 minutes to breathe in all the medicine. If a child cries or is uncooperative, they cannot receive all of the prescribed medication. During treatment, it’s important to assist your child be as still and calm as possible.
What are Nebulizers and Inhalers Used For?
Nebulizers and Inhalers are used to treat lung conditions like COPD and Asthma. They assist in getting medicine into the lungs. Breathing becomes simpler and the airways are opened with the use of inhaled drugs. Medication administered intrapulmonary (IV) facilitates a quicker onset of action compared to oral administration. Inhaling medication also helps lower the risk of many common medication side effects, like upset stomach or nausea.
You can also use inhalers and nebulizers to prevent or reduce the frequency of your symptoms. For instance, if you have Asthma, you might use an inhaled medication every day to assist in preventing Asthma attacks. If you have COPD, using a nebulizer or inhaler can help you breathe more easily and avoid flare-ups.
5 Tips For Using Inhaled COPD Medicine
- Know how to use it: Inhaled medication is useless if not used properly. Discuss the directions with your physician, pharmacist, or, if you own a nebulizer, a representative of the medical supply company as soon as you receive the prescription. After that, check in sometimes to make sure that you’re still using it properly.
- Know when to use it: If your doctor prescribes an inhaler or nebulizer, make sure you understand when to use it. Is it only for times when you have a COPD flare-up? Or do you need it every day?
- Know how much you need: Always take the medication precisely as directed. Never take more or less than is advised by your physician. Don’t take more medication if it doesn’t assist during a flare-up of your COPD. Instead, seek immediate medical attention.
- Know what the drug does: You may require multiple types of inhalation medications. A bronchodilator, which eases the muscles around the airways and permits them to widen, is the most often used treatment for COPD. there are many types of Bronchodilators. Inhaled corticosteroids, which help reduce airway edema, are sometimes prescribed to treat COPD in certain patients. Some of these medications are short-acting. Others are long-acting, and some kick in quickly, while others take time to work.
What are The Side Effects of a Nebulizer VS. Inhaler?
Nebulizer and inhaler side effects are typically not too dissimilar. This is so because inhalers and nebulizers are gadgets rather than prescription drugs. The drug breathed with the device primarily determines the negative effects. For example, an Albuterol nebulizer is expected to have the same side effects as an Albuterol inhaler. Albuterol side effects include rapid heartbeat, sore throat, and Tremors. A fungal infection in the mouth known as oral thrush can be brought on by corticosteroid-containing nebulizers or inhalers. If you take one of these drugs via inhalation, your doctor may advise you to rinse your mouth to help avoid this side effect.
However, the face mask that comes with many nebulizers can raise the risk of unique side effects. During a treatment, the nebulizer mist may occasionally adhere to your skin, nose, or eyes. This could then cause side effects in these areas. Nebulizer parts must also be cleaned regularly to avoid the accumulation of bacteria or fungi. Infections may result from neglecting to clean them.
Can You Use a Nebulizer and Rescue Inhalers?
Nebulized drugs occasionally have the same components as rescue inhalers. You wouldn’t utilize them in tandem in this scenario. For instance, you normally wouldn’t use an albuterol rescue inhaler and nebulizer simultaneously. You may be more susceptible to adverse consequences as a result.
If your nebulizer contains a different medication than your rescue inhaler, you might be instructed to use them both. Dr. Sheetu Singh will give you instructions about using an inhaler and nebulizer together if that’s what they recommend.