Pulmonary rehabilitation plays a crucial role in the management of Chronic Obstructive Pulmonary Disease (COPD), significantly enhancing a patient’s quality of life. This all-inclusive program offers nutritional guidance, psychological support, instruction on lung health, and fitness training. Patients with COPD often have compromised cardiovascular fitness, muscle strength, and endurance; these can be improved with specialized exercise routines. Education sessions empower patients with knowledge about their condition, teaching them how to manage symptoms, use medications effectively, and avoid triggers. Nutritional guidance helps maintain a healthy weight, crucial for lung function. Furthermore, psychological assistance promotes overall well-being by addressing the anxiety and depression that sometimes accompany chronic conditions. Pulmonary rehabilitation helps people with COPD become more independent and have a higher quality of life by including these factors in addition to symptom relief and fewer hospital stays.
Dr. Sheetu Singh, a renowned expert in respiratory medicine, offers invaluable insights into the role of pulmonary rehabilitation in managing Chronic Obstructive Pulmonary Disease (COPD). She emphasizes the significance of customized exercise regimens that improve muscular strength and cardiovascular fitness, both of which are frequently compromised in COPD patients. She supports thorough instruction on managing the condition, which should include how to take medications correctly and prevent exacerbations.
Dr. Sheetu Singh also highlights the significance of nutritional counseling and psychological support in improving overall health and quality of life. By emphasizing these essential components, her recommendations highlight how pulmonary rehabilitation helps patients live more active and satisfying lives despite their chronic disease while also reducing symptoms and hospitalizations.
What is Pulmonary Rehab for COPD?
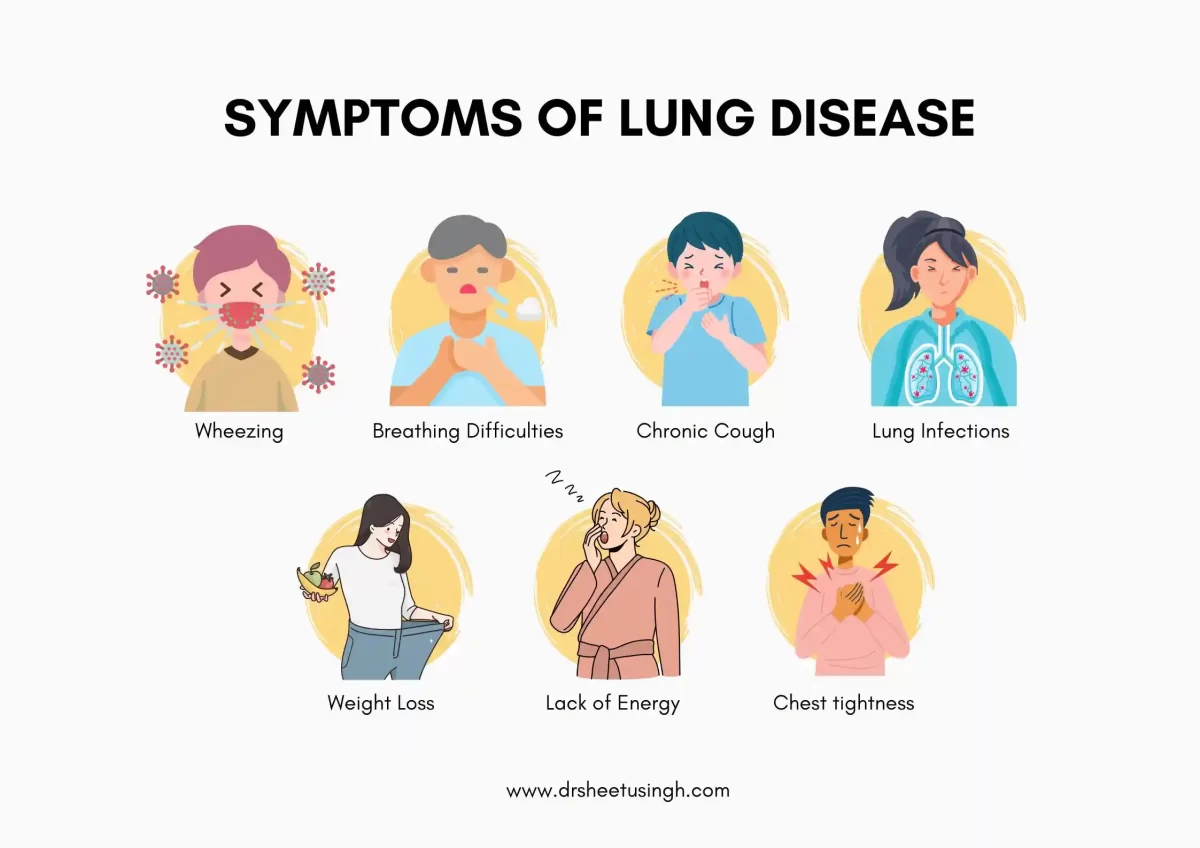
It can become more difficult to perform daily tasks like walking or climbing stairs if you have chronic obstructive pulmonary disease or COPD. That’s where pulmonary rehabilitation comes in.
It’s essentially an official program designed to improve your breathing and increase your level of fitness. Pulmonary Rehab will assist you with the following:
- Exercise.
- Nutrition.
- Breathing Techniques.
- Emotional and group support.
- Relaxation.
- Learning more about your medications.
A medical professional referral and proof of COPD diagnosis within the previous year are likely prerequisites for program enrollment. A group of experts, from social workers to nutritionists, may consult with you to determine the best course of action for your situation.
- Exercise
Exercise is essential to any pulmonary rehab program for COPD patients since it improves heart and lung function. Here are some more details regarding these exercises, which can be performed in a group or one-on-one with a trainer:
- Lower Body: Leg workouts are the main focus of the exercise program offered by most rehab facilities. They range from easy strolls around a track or on a treadmill to more strenuous stair climbing. The majority of pulmonary rehabilitation’s established advantages are demonstrated in studies using leg exercises.
- Upper Body: The muscles in the upper body are important for breathing, as well as for daily activities. Exercises for the arms and chest can include simply lifting your arms against gravity or rotating a crank against resistance.
- Breathing: You can strengthen your breathing muscles by forcing air through a mouthpiece against resistance. These exercises may be helpful for people with very weak breathing muscles.
- Strength Training: The majority of pulmonary rehab exercises concentrate on increasing stamina. It has also been demonstrated that adding strength exercises, such as lifting weights, is beneficial.
Educate Yourself
Group or individual education sessions are provided by many pulmonary rehab programs to assist you in learning how to effectively manage your COPD. Sessions might focus on things such as:
- Recognizing the treatment plan for your medication. This entails consistently and correctly using your inhaler.
- How to get the most out of oxygen therapy if you are using this treatment.
- If you’re a smoker, help with quitting.
- Eating a healthy diet.
Emotional Support
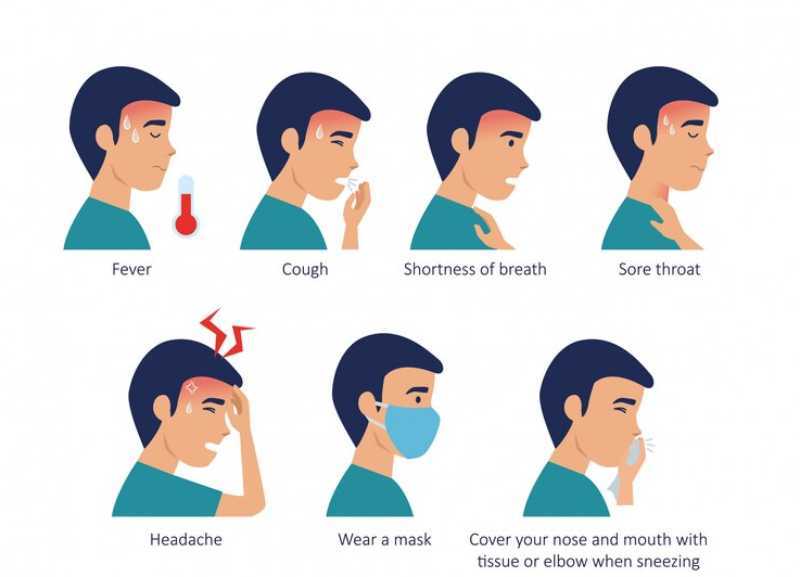
Anxiety or depression are common in people with severe COPD. You can become less interested in enjoyable pursuits as a result, including intimacy. Some pulmonary rehab programs offer relaxation training and counseling. Additionally, you’ll have the opportunity to talk about your concerns and issues with other COPD patients.
What You Get Out of a Program
Most people who finish a pulmonary rehab course feel better at the end. Generally, you can accomplish more without running out of breath. In a thorough examination of certain programs, almost every patient receiving pulmonary rehabilitation reported improved symptoms.
- Less Short of Breath.
- More Energetic.
- More in Control of their COPD.
What is the role of Pulmonary Rehabilitation?
- In COPD, pulmonary rehabilitation (PR) is a crucial management approach.
- Interdisciplinary program.
- Personalized and uniquely created
- Optimizes the autonomy, and social and physical performance of each patient.
Objectives of Pulmonary Rehabilitation?
The primary goal of pulmonary rehabilitation is to manage the secondary morbidities.
- Physical inactivity.
- Malnutrition.
- Myopathy.
- Depression.
- Osteoporosis.
When Should Pulmonary Rehabilitation Start?
- Non Symptomatic Smoker.
- Symptomatic COPD Patients.
- COPD Exacerbation
- Respiratory Failure
Contraindications and Barriers to Pulmonary Rehabilitation
- Lack of motivation and adherence.
- Psychiatric illness.
- Dementia.
- Uncontrolled cardiovascular diseases.
- Excessive physical activity-induced hypoxia that is not oxygenated
- Not being able to exercise (because of orthopedic or other issues).
- Additional unstable illnesses, such as diabetes and hepatic.
- Severe PH, CLD, AKI, AECOPD
Exercise for Pulmonary Rehabilitation
- Three primary areas, aside from general exercise
- Breathing exercises
- Upper limb exercises
- Lower limb exercises
- There are two sorts of workouts in each of these areas:
- Strength: High weight, low repetition
- Endurance: Low weight, high repetition
FAQs
What is pulmonary rehabilitation?
A thorough program called pulmonary rehabilitation is intended to assist individuals with long-term lung conditions like COPD in enhancing their general quality of life, emotional stability, and physical fitness. It includes education on lung health, exercise training, nutritional counseling, and psychological support.
How does pulmonary rehabilitation benefit COPD patients?
Patients with COPD benefit from pulmonary rehabilitation because it increases their muscle strength, endurance, and cardiovascular fitness. Additionally, it offers instruction on how to successfully use drugs, manage symptoms, and stay away from triggers. Nutritional counseling and psychological support further enhance overall health and well-being.
What types of exercises are included in pulmonary rehabilitation?
Aerobic exercises such as walking or cycling, strength training to increase muscle endurance, and breathing exercises to improve lung function are frequently included in the exercise component of pulmonary rehabilitation. These exercises are tailored to each patient’s fitness level and specific needs.
How long does a pulmonary rehabilitation program last?
A standard pulmonary rehabilitation program consists of two or three sessions each week for a duration of around eight to twelve weeks. The duration can vary based on individual programs and specific health goals.
Can pulmonary rehabilitation prevent COPD exacerbations?
Yes, Pulmonary Rehabilitation can assist reduce the frequency and severity of COPD exacerbation by improving overall physical conditioning, teaching effective symptom management strategies, and promoting better adherence to treatment plans.