How to Treat Asthma Triggered by Cold Weather: During the winter, breathing cold air can aggravate asthma symptoms. If you have Asthma, you may find that your symptoms are affected by the seasons. Walking outside during colder months can exacerbate breathing difficulties. Furthermore, exercising in the cold can exacerbate symptoms like wheezing and coughing even more quickly.
What’s the Connection Between Cold Weather and Asthma?
When you have asthma, certain triggers cause your bronchial tubes, which are responsible for your airways, to expand and become irritated. Swollen airways are narrower and can’t take in as much air. This explains why breathing difficulties are a common symptom of asthma in humans. Winter is a particularly challenging season for asthmatic individuals. According to a 2014 Chinese study, hospital admissions for asthma increased in the winter. Furthermore, up to 82% of asthmatics who exercised in the chilly northern environment of Finland reported having trouble breathing.
When you work out, your body needs more oxygen, so your breathing speeds up. If you want to breathe in more air, you frequently do it through your mouth. Direct airflow through your mouth leaves the air chilly and dry, whereas air passing through your nose has blood vessels that warm and humidify the air before it reaches your lungs. Exercising outdoors in cold weather delivers cold air rapidly to your airways. It also seems to make you more likely to get an asthma attack.
Why Does Cold Air Affect Asthma Symptoms?
Asthma symptoms are exacerbated by cold air for various reasons.
1. Cold Air is Dry: Your airways are lined with a thin layer of fluid. That fluid evaporates faster than it can be replenished when you breathe in dry air. Asthma symptoms develop when dry airways become inflamed and swollen.
The same molecule that your body produces during an allergy attack, called histamine, is also released into your airways by cold air. Histamine triggers wheezing and other Asthma symptoms.
2. Cold Increases Mucus: Additionally, a coating of protective mucus lines your airways, aiding in the removal of harmful particles. In cold weather, your body produces more mucus, but it’s stickier and thicker than normal. Your risk of getting a cold or other infection is increased by the excess mucus.
3. You’re More Likely to Get Sick or be Indoors When it’s Cold: Winter is when colds, the flu, and other respiratory illnesses are most common. It is also known that these infections trigger asthmatic symptoms. Cold air can also drive you indoors, where mold, dust, and pet dander flourish. For certain people, these allergens cause asthma symptoms.
What Precautions Should People with Asthma Take?
Before winter approaches, make sure your asthma is under control. After creating an asthma action plan with Dr. Sheetu Singh, take the prescribed medications. You may take medicine every day (for long-term control) or just when you need it (for quick relief). Medications known as long-term controllers are taken daily to treat symptoms of Asthma. They include:
- Inhaled corticosteroids—like fluticasone—are found in Flovent Diskus and Flovent HFA.
- long-acting beta-agonists, including Serevent Diskus Salmeterol.
- Leukotriene modifiers, such as Montelukast (Singulair).
Only take quick-relief medications when necessary, like before working out in the cold. Anticholinergics and short-acting Bronchodilators are examples of these drugs.
How Can You Avoid Asthma Attacks in the Cold?
Try to stay inside during extremely low temperatures, especially if it’s below 10°F (-12.2°C), to avoid asthma episodes. If you do have to go outside, cover your mouth and nose with a scarf to warm the air before you breathe it in. Here are a few other tips:
- During the winter, consume more fluids. This may make the mucus in your lungs thinner, making it simpler for your body to expel.
- Get your flu vaccine early in the fall.
- Try to avoid anyone who appears to be sick.
- To get rid of dust mites, wash your blankets and sheets in hot water once a week.
- To get rid of indoor allergens, dust and vacuum your house frequently.
Here are some ways to prevent Asthma attacks when you exercise outdoors in cold weather:
- Before you work out, give your inhaler a 15 to 30-minute run. This facilitates simpler breathing by widening your airways.
- In case you experience an Asthma attack, always keep an inhaler on hand.
- Before working out, spend at least ten to fifteen minutes warming up.
- Wear a scarf or mask over your face to warm the air you breathe in.
What Else Can Cause an Attack?
One of the major asthma triggers is the cold. Additional triggers for your symptoms could be:
- Strong scents.
- Allergens such as mold, pollen, animal dander, and dust mites.
- Tobacco smoke.
- Stress.
- Exercise.
- Bacterial or viral infections.
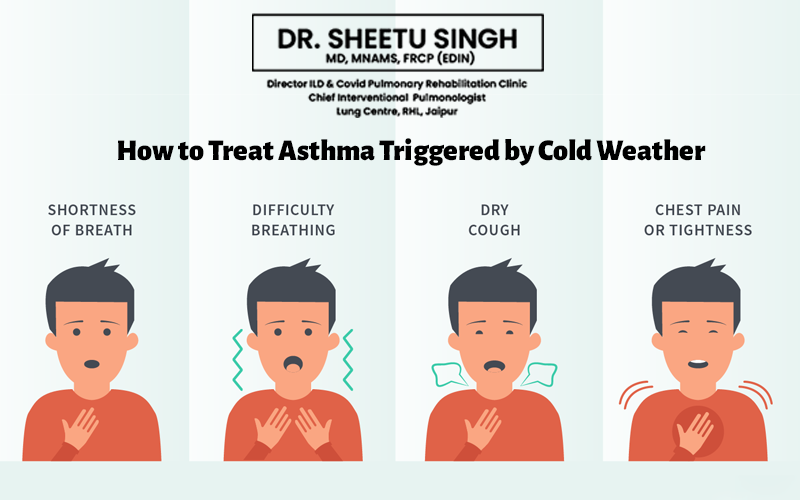
What are the Symptoms of an Asthma Attack?
When you have symptoms like these, you know you’re experiencing an asthma attack:
- Coughing.
- Shortness of breath.
- Pain or tightness in your chest.
- Wheezing.
- Trouble speaking.
What Can You Do if You’re Having an Asthma Attack?
Consult Dr. Sheetu Singh and the asthma action plan you created if you begin to wheeze or feel out of breath. Take your quick-acting medication and get medical help right away if your symptoms are so bad that you are unable to speak. You may need to stay in observation until your breathing stabilizes. Additional general advice on what to do in the event of an asthma attack is provided below:
- Utilizing a quick-acting rescue inhaler, take two to six puffs. Your airways should be cleared by the medication, making breathing simpler for you.
- Nebulizers can potentially be a viable substitute for inhalers. A nebulizer is a device that creates a tiny mist for you to breathe in while taking your medication.
- If your symptoms aren’t severe but they don’t improve with the first few puffs from your inhaler, wait 20 minutes and then take another dose.
- Give your doctor a call once you’re feeling better. Your quick-acting medication may need to be taken every few hours for a couple of days.
