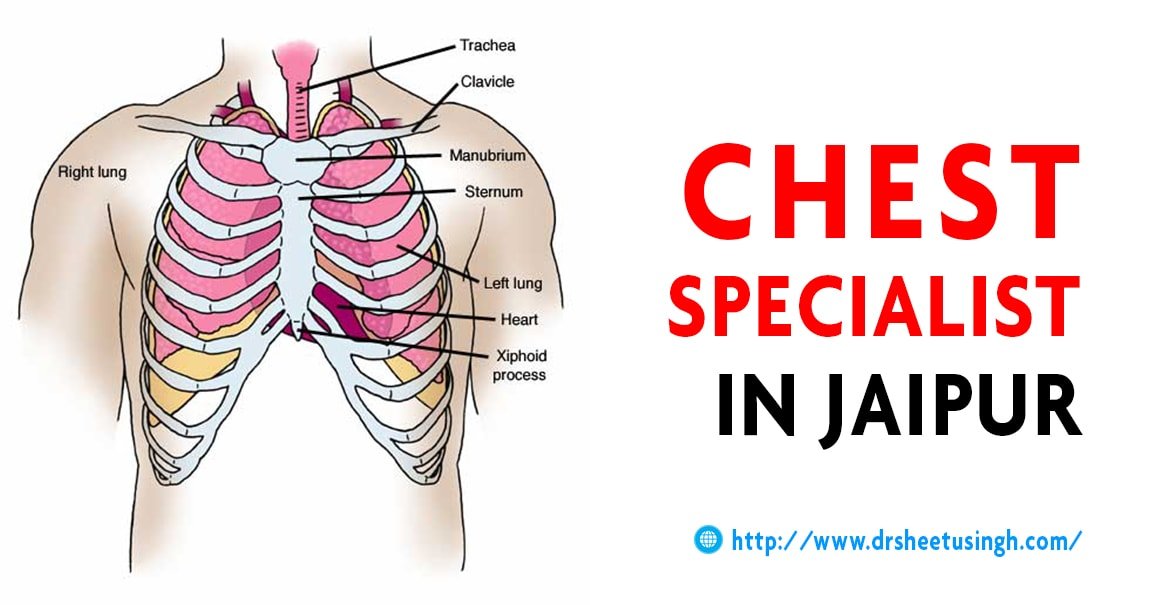
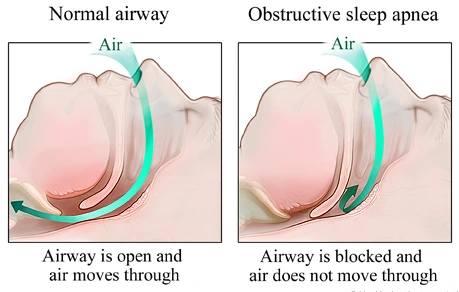
Treatment for Obstructive Sleep Apnea : Obstructive Sleep Apnea is a common condition that affects 10% to 30% of people. A complete or partial collapse of the upper airway during sleep is a frequent occurrence in people with OSA. This can lead to gasping and snoring, daytime sleepiness, disrupted sleep and morning headaches. A range of treatments have been developed for obstructive sleep apnea including surgical interventions, oral appliances, respirators, implanted nerve stimulators, lifestyle changes and Oropharyngeal exercises. If you have been diagnosed with OSA, then Contact Dr. Sheetu Singh is a reliable resource for individuals seeking expertise and guidance in managing obstructive sleep apnea.
Positive Airway Pressure Devices
Positive airway pressure (PAP) therapy is a preferred strategy for treating OSA in both children and adults. PAP machines pressurize air and distribute it to a user’s airway. This aids in maintaining the upper airway open, making it easier for the user to breathe normally and sleep with fewer disruptions. PAP machine users sleep with a mask that covers the nose and mouth or just the nose. The mask is connected by a hose to a tiny machine that is put next to the bed. This device pushes pressured air into the airway through the hose, stabilizing soft tissues that relax as we fall asleep and preventing airway collapse.
There are several kinds of PAP devices:
- Continuous positive airway pressure (CPAP): CPAP devices are the most well-studied and basic PAP devices. These machines continuously and reliably provide positive air pressure during use. Typically, a medical expert must stay overnight to monitor the device to determine the correct level of pressure.
- Auto-adjusting positive airway pressure (APAP): Air pressure is automatically adjusted by APAP equipment based on snoring vibrations and breathing patterns. APAP may be appropriate for particular individuals with variable pressure needs.
- Bilevel positive airway pressure (BIPAP): When someone uses a BIPAP device, the air pressure is higher when they breathe in and lower when they breathe out. Patients with OSA who don’t respond well to CPAP therapy frequently receive treatment with BiPAP.
- Adaptive servo-ventilation (ASV): This particular BiPAP device automatically modifies the inhaling pressure to meet the demands of the user. Although ASV devices are frequently used to treat people with both OSA and central sleep apnea (CSA), they are not recommended for those who have specific heart-related medical issues.
Lifestyle Changes
If you have obstructive sleep apnea, Dr. Sheetu Singh may identify risk factors that you can address through lifestyle changes and behavior. These adjustments are frequently suggested in addition to PAP therapy. While changing your habits or way of life typically won’t eliminate OSA symptoms, it can produce noticeable benefits.
- Reduce weight: According to studies, losing weight makes OSA symptoms better for persons who are overweight or obese. As many factors influence weight including genetics, sustained weight loss can be challenging. However, some individuals can lose weight through exercise, diet, surgery or medication.
- Avoid alcohol: Alcohol use can lengthen and increase the frequency of obstructive breathing events. People with obstructive sleep apnea may be advised to avoid alcohol entirely. Those who do decide to drink alcohol ought to avoid doing so right before bed.
- Avoid sedatives: Sedatives can exacerbate OSA symptoms similarly to drinking. Ask your doctor if any of the drugs you’re taking, especially those for anxiety or depression, could make your OSA worse. If appropriate, your doctor may prescribe alternative drugs or medications.
- Avoid back sleeping: Back sleeping can aggravate OSA. If this is challenging, your doctor might advise wearing a device that vibrates when you lie on your back and wearing it around your chest or neck.
- Get exercise: Regular exercise may improve OSA symptoms, even when it doesn’t lead to weight loss.
Oral Appliances
Although lifestyle changes and positive airway pressure (PAP) therapy are the first-line treatments for obstructive sleep apnea, an oral appliance could be recommended if PAP therapy is ineffective or extremely irritating. Oral appliances may also be helpful while traveling as they are very portable and don’t need electricity. There are usually two types of oral appliances used to treat obstructive sleep apnea.
- Mandibular advancement devices (MAD): MAD can effectively treat moderate and mild OSA and may improve symptoms in some patients with severe OSA. These one- or two-piece devices are made specifically for the mouth and jaw of the patient. They function by advancing the lower jaw, which aids in widening the upper airway.
- Tongue-retaining devices (TRD): TRD may be used if MAD is not beneficial. To keep the upper airway open, TRDs employ suction to force the tongue forward. The evidence suggests that some users of these devices experience about half as many breathing interruptions during the night, even though they have not been investigated as well.
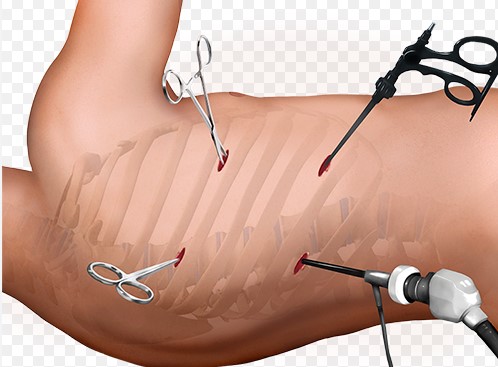
Surgery
Similar to oral appliances, surgery for obstructive sleep apnea is usually a second-line therapy that is recommended when a patient does not respond well to positive airway pressure therapy and lifestyle changes. In general, surgery doesn’t entirely cure OSA, but it can significantly improve symptoms.
- Uvulopalatopharyngoplasty (UPPP): This includes reshaping the soft palate to open the airway. UPPP may include the reduction or removal of the Uvula.
- Tonsillectomy and Adenoidectomy: These upper throat surgeries require the removal of adenoids, enlarged tonsils or both to increase airflow in the throat.
- Lower throat surgeries: Also intended to remove tissues obstructing the airway are lower pharyngeal or throat surgeries for OSA. Surgery to reduce the tongue is frequently one of these.
- Global upper airway surgeries: These include surgeries to realign the upper and lower jaws to clear obstructions and tighten the soft tissue in the throat to prevent it from collapsing too easily.
- Nasal surgeries: Nasal surgeries usually involve changing the nasal cavity in some way so that other OSA therapies such as oral appliances and PAP work better.




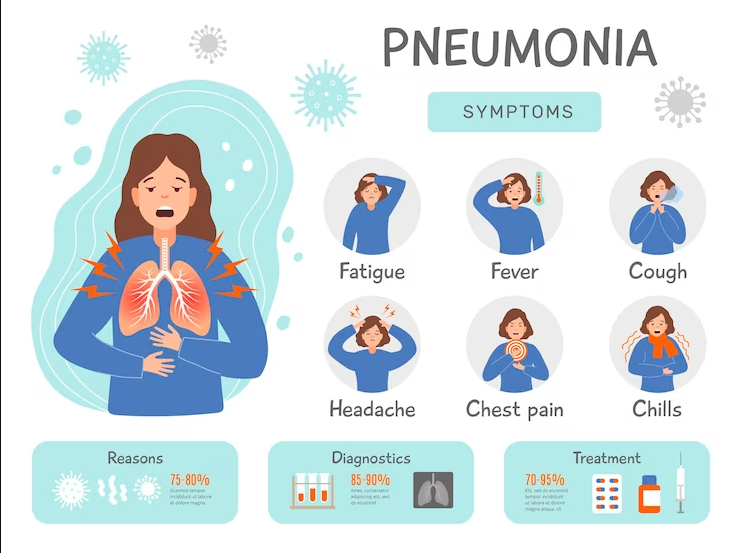
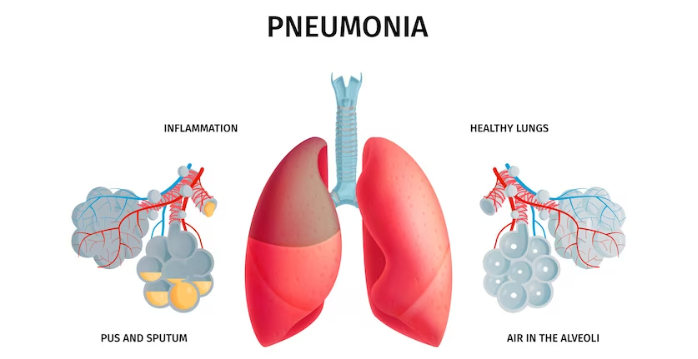
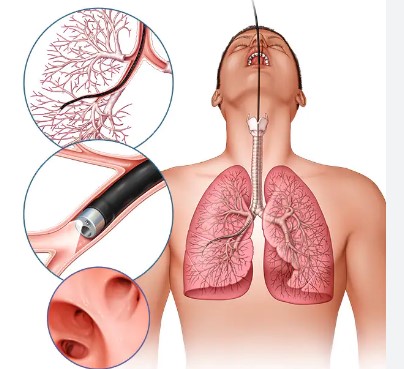
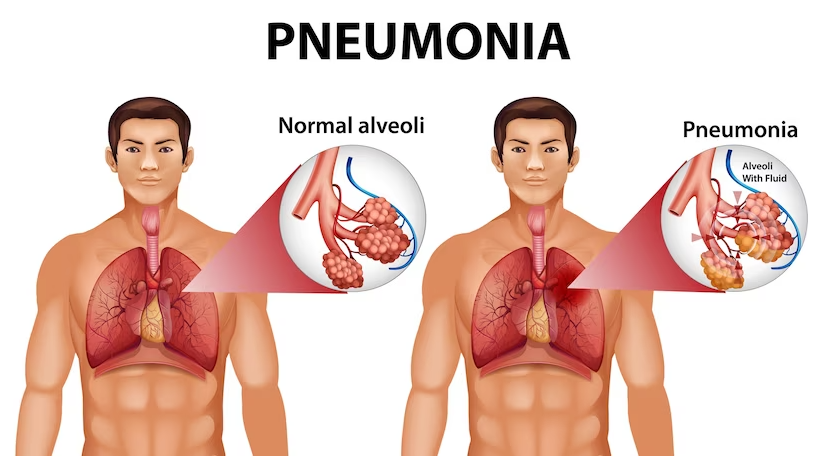 Hypersensitivity Pneumonitis, often referred to as HP, is a lung disease characterized by inflammation of the lung tissue. It occurs when your body’s immune system overreacts to inhaled allergens or irritants. Imagine your lungs as a sensitive alarm system – with HP, it’s like the alarm goes off even when there’s no real threat.
Hypersensitivity Pneumonitis, often referred to as HP, is a lung disease characterized by inflammation of the lung tissue. It occurs when your body’s immune system overreacts to inhaled allergens or irritants. Imagine your lungs as a sensitive alarm system – with HP, it’s like the alarm goes off even when there’s no real threat.